- Online Patient Services
- Patient Booklet
- e - Medical Records
- Online Expert Opinion-NAVYA
- Donation to TMC
- Online Hospital Statistics
- Pensioner Portal
- Travel Facility
- Schedule of Charges
- FAQs
- International Patients Advisor
- TMC - Annual Report
- TMC -Performance Statistics
- TMH Facts: average per day
- Classification of Surgeries
- D.A.E
- Govt of India Sites :
- International Affiliations
- Pancreatic Cancer India
- Tobacco Act
- Observership Application
- Teleconsulting Services
- टीएमसी
- होम
- हमारे बारे में
- मरीज सेवायेँ
- कैंसर संबंधी जानकारी
- विभाग
- एनसीजी
- रोग प्रबंधक वर्ग
- शिक्षण एवं अनुसंधान
- घटनायें
Department of Radiodiagnosis
- About Us
- Department Activity
- Education & Courses
- Research
- Patient Information
- Online Quiz
- Contact Us
Radiography (X-Rays) (CR and DR)
 In addition to routine radiography of the chest, abdomen and bones, a large number of specialized procedures such as Orthopantomograms (OPG), as well as procedures employing contrast media such as Barium studies, intravenous urography (IVU), Cysto-urethrograms, Angiograms, Sialograms, etc are carried out in the Radiodiagnosis department. All routine radiography is performed using the Computed Radiography (CR) and Digital Radiography (DR) systems and the radiographs of chest, bones, etc., as well as contrast procedures are acquired in the digital format and stored in the PACS (Picture Archiving and Communication System). With the use of Digital Radiography system, x-rays are immediately seen on the monitor of DR and can be viewed immediately by the treating physicians and aid them in patient care. The reporting of these investigations is done directly on the high resolution Workstation Monitors (soft copy reporting).
In addition to routine radiography of the chest, abdomen and bones, a large number of specialized procedures such as Orthopantomograms (OPG), as well as procedures employing contrast media such as Barium studies, intravenous urography (IVU), Cysto-urethrograms, Angiograms, Sialograms, etc are carried out in the Radiodiagnosis department. All routine radiography is performed using the Computed Radiography (CR) and Digital Radiography (DR) systems and the radiographs of chest, bones, etc., as well as contrast procedures are acquired in the digital format and stored in the PACS (Picture Archiving and Communication System). With the use of Digital Radiography system, x-rays are immediately seen on the monitor of DR and can be viewed immediately by the treating physicians and aid them in patient care. The reporting of these investigations is done directly on the high resolution Workstation Monitors (soft copy reporting).
Digital Mammography with Tomosynthesis
 Mammography is performed on the state of art GE Senograph DS Full Field Digital Mammography unit and Hologic Full Field Digital Mammography with Tomosynthesis, which provides unsurpassed image quality at minimal radiation dose. Soft copy reporting of the digital images is done on the attached high resolution Workstations. The workstation is also equipped with Computer Aided Detection (CAD) software which assists the radiologists in detecting small masses and microcalcifications in the breasts.
Mammography is performed on the state of art GE Senograph DS Full Field Digital Mammography unit and Hologic Full Field Digital Mammography with Tomosynthesis, which provides unsurpassed image quality at minimal radiation dose. Soft copy reporting of the digital images is done on the attached high resolution Workstations. The workstation is also equipped with Computer Aided Detection (CAD) software which assists the radiologists in detecting small masses and microcalcifications in the breasts.
Special Procedure performed:
- Needle Localization
- Stereotactic Biopsy
Mammography and ultrasound guided needle biopsies and hook-wire localization procedures are performed in order to achieve a definitive diagnosis in nonpalpable cases of breast cancer. Tomosynthesis is performed on the Hologic Full Field Digital Mammography machine.
Tomosynthesis can reduce or eliminate the tissue overlap and hence the summation artifacts. It also solves the problem of superimposition and helps in detection of obscured cancer. It thus improves the sensitivity and specificity of mammography, especially in patients with dense breasts.
Ultrasound & Colour Doppler
 The Ultrasonography department is equipped with nine state of the art Ultrasound machines which contribute to the high level of confidence of the Radiologist for evaluation of the lesions and serve as excellent guiding tools for the various Diagnostic and Therapeutic procedures. All ultrasound machines as well as operators are registered under PCPNDT act. Sex determination is not performed in our department.
The Ultrasonography department is equipped with nine state of the art Ultrasound machines which contribute to the high level of confidence of the Radiologist for evaluation of the lesions and serve as excellent guiding tools for the various Diagnostic and Therapeutic procedures. All ultrasound machines as well as operators are registered under PCPNDT act. Sex determination is not performed in our department.
Four machines are used for the diagnostic purposes to carry out various ultrasound examinations of the abdomen, pelvis and small parts, as well as intracavitary (transrectal and transvaginal) examinations.
Tissue Harmonic Imaging helps for high resolution at depth and the Cross Beam Imaging facility makes the lesion to stand out with better border delineation.
The 3D Application further helps to better understand relations of the lesion with organs in the vicinity and the Biopsy Attachment helps in precisely targeting the lesion.
The Color Doppler scanners are extensively used to assess the vascularity of the tumors. The arterial and venous Doppler examinations are carried out for the evaluation of patients with associated peripheral Vascular Diseases and screening as well as diagnosis of the Deep Venous Thrombosis.
A registry is maintained in the Ultrasound section for the patients with Venous Thromboembolic Disease as a part of the Thrombosis Management Group Activity.
The Ultrasound Equipment in the Interventional Radiology Unit is an integral part of the set up as it serves as an important guide for the Vascular as well as Non-vascular procedures for access and precise placement of the needles.
The portable Ultrasound unit delivers the conveniences and versatility with its application in:
- The ICU for Emergency Scanning of ICU patients
- Bedside Drainage procedures like
- Pleural & Peritoneal Tapping
- Abscess Aspiration
- Indwelling Pigtail Drainage
Intraoperative Ultrasound Scanning facility is provided to facilitate
- Resection of the tumors by localization of small lesions
- To assess vascular involvement intraoperatively
- To assess complete removal of the lesion
- To perform Intraoperative Tumor Ablation (Radiofrequency Ablation)
Ultrasound evaluation of Breast lesions in conjunction with mammography contributes in the diagnosis of
- Isodense lesions
- Imaging of dense breast
- Young glandular breast
- Differentiating between solid and cystic lesions
- Differentiating between post op seroma and recurrent masses.
Computerized Tomography ( CT Scan )
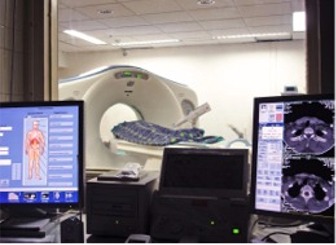 Multi-slice CT scan is one of the most potent tools for the early detection, diagnosis and treatment planning of cancer. CT scanning of the whole body is carried out on the GE Lightspeed 16 Multislice CT scanner and SIEMENS Somatom emotion 16 Multislice CT scanner, which is capable of obtaining 16 slices per rotation of the x-ray tube. Dual / Triple phase contrast enhanced scans, Dynamic scans, CT Angiography, and 3D reformations are carried out wherever applicable. Multiplanar reformatted images are routinely obtained on the diagnostic workstations to aid in the diagnostic interpretation of the CT scans.
Multi-slice CT scan is one of the most potent tools for the early detection, diagnosis and treatment planning of cancer. CT scanning of the whole body is carried out on the GE Lightspeed 16 Multislice CT scanner and SIEMENS Somatom emotion 16 Multislice CT scanner, which is capable of obtaining 16 slices per rotation of the x-ray tube. Dual / Triple phase contrast enhanced scans, Dynamic scans, CT Angiography, and 3D reformations are carried out wherever applicable. Multiplanar reformatted images are routinely obtained on the diagnostic workstations to aid in the diagnostic interpretation of the CT scans.
Special Services Offered
1. CT Angiography
2. CT Perfusion
3. CT Cholangiography
4. Virtual Colonoscopy
5. Virtual Bronchoscopy
6. CT Enteroclysis
7. CT Arterioportogram
8. CT Guided Procedures:
* CT guided Biopsies
* CT Guided Drainage Procedures
* CT Guided Tumor Ablation (Radiofrequency Ablation [RFA] and Microwave Ablation [MWA])
* CT Guided Nerve Blocks
* CT Guided Sclerotherapies
9. Dentascan
10. 3D Reconstruction image
11. Multiplanar Reconstruction
Magnetic Resonance Imaging ( MRI )
 Magnetic Resonance Imaging of the whole body is performed in our department on the GE Signa 1.5 Tesla MRI and Philips Ingenia 1.5 tesla MRI systems, using a variety of pulse sequences including ultra-fast sequences. The majority of MR imaging studies are of the brain, head, neck, spine and musculo-skeletal system; followed by MR imaging of the abdomen and pelvis, breast and other specialized investigations like MR Cholangio-pancreatography, cisternography and myelography. MR studies of the pelvic organs, especially the uterus and cervix, and of the prostate are also carried out. MR Angiography of abdominal, neck and intracranial blood vessels as well as of musculoskeletal system is also performed whenever indicated.
Magnetic Resonance Imaging of the whole body is performed in our department on the GE Signa 1.5 Tesla MRI and Philips Ingenia 1.5 tesla MRI systems, using a variety of pulse sequences including ultra-fast sequences. The majority of MR imaging studies are of the brain, head, neck, spine and musculo-skeletal system; followed by MR imaging of the abdomen and pelvis, breast and other specialized investigations like MR Cholangio-pancreatography, cisternography and myelography. MR studies of the pelvic organs, especially the uterus and cervix, and of the prostate are also carried out. MR Angiography of abdominal, neck and intracranial blood vessels as well as of musculoskeletal system is also performed whenever indicated.
MR Proton Spectroscopy is employed in selected cases for evaluation of brain tumours or other lesions, using both the single voxel and multi-voxel spectroscopy available in our systems. MR Perfusion studies for the brain are also performed in our department for evaluation of suspected primary or recurrent brain tumours.
Diffusion tensor imaging (DTI) and Functional MR imaging are also performed in our department in pre op assessment of certain brain tumors and to aid surgeons in surgical planning.
With its exquisite soft tissue contrast, MR is the imaging modality of choice to investigate cancers of the various parts of body.
Picture Archival And Communication System ( PACS )
 Images from the digital imaging modalities i.e. CT, MRI, Ultrasound, Radiography (CR and DR), DSA and Digital Mammography, are stored in PACS (GE Centricity) and can also be transmitted across the hospital network so that as soon as the images are acquired by each of these modalities, they can be viewed by the referring physicians without any delay on the PC in their office, OPD, or any other site in the hospital. The Radiology report of each examination stored in the Radiology Information System (RIS) can also be viewed along with the corresponding images. Reporting of all Computed Radiography, CT, MRI, Ultrasound and Mammography examinations is carried out on the Diagnostic workstations (soft copy reporting), and routine filming of these examinations has been discontinued. The department is now completely filmless and films are only printed on request by the patient or referring physician.
Images from the digital imaging modalities i.e. CT, MRI, Ultrasound, Radiography (CR and DR), DSA and Digital Mammography, are stored in PACS (GE Centricity) and can also be transmitted across the hospital network so that as soon as the images are acquired by each of these modalities, they can be viewed by the referring physicians without any delay on the PC in their office, OPD, or any other site in the hospital. The Radiology report of each examination stored in the Radiology Information System (RIS) can also be viewed along with the corresponding images. Reporting of all Computed Radiography, CT, MRI, Ultrasound and Mammography examinations is carried out on the Diagnostic workstations (soft copy reporting), and routine filming of these examinations has been discontinued. The department is now completely filmless and films are only printed on request by the patient or referring physician.
Interventional Radiology
 The Interventional Radiology (IR) Unit of the department is a team of health care professionals committed to the cause of enhancing patient care by using advanced imaging technology. The patients are treated with minimally invasive and targeted therapies that help for early recovery and better quality of life of the patients. The various needles or catheter required to be placed deep in the body of the patients for diagnosis or treatment of the patient's disease are introduced precisely under the guidance of imaging modalities like Ultrasound, Digital Fluoroscopy, Digital subtraction Angiography, or CT Scan. Most of these procedures are done under Local Anesthesia and IV Sedation through a tiny incision in the skin. General anesthesia is given to pediatric patients and in patients in whom the procedure is painful if not anesthetized like Radiofrequency Ablation (RFA).
The Interventional Radiology (IR) Unit of the department is a team of health care professionals committed to the cause of enhancing patient care by using advanced imaging technology. The patients are treated with minimally invasive and targeted therapies that help for early recovery and better quality of life of the patients. The various needles or catheter required to be placed deep in the body of the patients for diagnosis or treatment of the patient's disease are introduced precisely under the guidance of imaging modalities like Ultrasound, Digital Fluoroscopy, Digital subtraction Angiography, or CT Scan. Most of these procedures are done under Local Anesthesia and IV Sedation through a tiny incision in the skin. General anesthesia is given to pediatric patients and in patients in whom the procedure is painful if not anesthetized like Radiofrequency Ablation (RFA).
The unit is well equipped with two Digital Subtraction Angiography (DSA) Machines, one CT scan (Siemens Somatom Sensation, 16 slice Multidetector system) and two Ultrasound Machines. The recently installed DSA machine the 'INNOVA IGS 540’ is state of the art equipment that gives very high resolution angiography Images with the 3D Rotational angiography at reduced patient dose. Also with the unique 3D CT acquisition facility on this DSA, Angiography and CT like imaging can be done on the same machine.
MIYABI (HYBRID CT – DSA) Equipment by Siemens has been installed in June 2013. CT Guided & Fluro Guided Interventional procedures can be performed in the same sitting. Vascular lesions can be evaluated with more precision and any intervention if needed can be planned in the same session. Cervical vertebroplasties where CT guidance for Needle Placement and Fluoroguidance for cement injection are required can be done. Combined Pain Management procedure like RFA (Radio Frequency Ablation) and osteoplasty can be done in same session. Combined Locoregional therapies like Radio Frequency Ablation with chemoembolisation can be performed. Skull bone intervention will be more precise & safe.
EMERGENCY SERVICES PROVIDED
Diagnostic/Non invasive-
- X-rays
- Ultrasonography (USG)
- Computed Tomography (CT) scan
- CT angiogram
Invasive-
- USG guided pleural/ascitic fluid tapping and pigtailing
- USG guided drainage and pigtailing of abscess and collection
- CT guided drainage of abscess and collection
- Fluoroscopy guided drainage Procedures for Cholangitis , Obstructive Uropathy, etc.
- Angiography & Embolisation for Gastrointestinal Bleeding, Hemoptysis , Hematuria , Tumor Bleed , Intra/ Post Operative Bleeding, etc.
Interventional Procedures
Diagnostic Procedures
- Ultrasound Guided Fine Needle Aspiration cytology (FNAC) and Biopsy
- CT Guided FNAC and Biopsy
- Endobronchial Ultrasound (EBUS) Guided Biopsy
- Diagnostic aspiration of ascitic or pleural fluid for cytology
- Therapeutic aspiration of ascitic and pleural fluid
- Diagnostic Angiographies
- Transjugular Liver Biopsy
- Liver resection planning and FLR assessment
- Lymphangiography
Therapeutic Procedures
Head and Neck
Non Vascular
- Fluoro guided BOTOX injection in post laryngectomy patient
- Direct puncture embolisation of tumors
Vascular-
- Superselective ophthalmic artery Chemoinfusion for Intra-ocular retinoblastoma
- Balloon test occlusion for skull base tumors
- Intra-arterial thrombolysis
- Intracranial venous sinus thrombolysis
- Angioplasty
- Stenting and coiling of intracranial aneurysm
- Pre-operative arterial embolisation of skull base tumor
- Sclerotherapy and angioembolisation for arterio-venous malformation
Thoracic
Non Vascular
- Radiofrequency ablation of pulmonary neoplastic lesions
- Pre-operative wire localisation of lung nodules
- Chest tube placement
- Drainage of pleural effusion or collection
- Tracheo-bronchial stenting
- Pleural and bronchial leak occlusion
- Fluoro guided port insertion
- Indwelling tunnel catheter placement for pleural fluid
- Lymphangiography and lymphatic Embolisation
Vascular-
- Pulmonary arteriogram and venogram
- Pulmonary artery thrombolysis
- Pulmonary Embolectomy
- Bronchial artery embolisation
- Pre-operative embolisation of tumors
- Foreign body retrieval
- Central venous line placement, i.e., PICC line insertion, Hickman insertion, port placement
Hepatic and Gastrointestinal
Non Vascular-
- Biliary Drainage – external
- Biliary Drainage – internal/external
- Biliary Drainage – internal metal stent placement
- Ethanol / Acetic Acid Sclerotherapy
- Fluid Collection / Abscess Drainage
- Intravascular foreign Body removal
- Percutaneous gastrostomy
- Percutaneous Jejunostomy
- Fluoro Guided Ryle’s tube insertion
- Fluoro Guided Naso-jejunostomy tube insertion
- Radiofrequency ablation of tumors
- Endobiliary Radiofrequency Abltion (Endobiliary RFA)
- Endobiliary Brachytherapy
- Microwave ablation
- Irreversible Electropolation
- Lymphangiography and lymphatic Embolisation
Vascular-
- Arteriogram, portogram and venogram
- Arterial Thrombolysis
- Angioplasty / Stenting
- Hepatic vein stenting
- IVC venoplasty/stenting
- Inferior Vena Cava Filter placement and retreival
- Transjugular Intrahepatic Portosystemic Shunt (TIPSS)
- Trans-arterial chemoembolisation of hepatic tumors with conventional lipiodol (Lipiodol TACE)
- Trans-arterial chemoembolisation of hepatic tumors with Dreg Eluting Beads (DEB-TACE)
- Trans-arterial Radioembolisation of hepatic tumor (TARE)
- Pre-operative embolisation of tumors
- Portal vein embolisation
- Embolisation in gastrointestinal bleeding
- Hepatic Venous Pressure Gradient measurement
Genitourinary
Non-Vascular
- Nephrostomy Drainage – external
- Nephrostomy Drainage – internal/external
- Nephrostomy Drainage – Internal "double J" stent
- Foreign Body removal
Vascular-
- Arteriogram and venogram
- Angioplasty / Stenting
- Arterial Thrombolysis
- Venous Thrombolysis
- Uterine Artery Embolisation (UAE)
- Pre-operative Embolisation of tumors
- Radiofrequency Ablation of tumors
- Microwave ablation of tumors
Musculoskeletal
Non-Vascular
- Osteoplasty
- Vertebroplasty
- Kyphoplasty
- Radiofrequency ablation of tumors
- Lymphangiography and lymphatic Embolisation
Vascular-
- Arteriogram and venogram
- Angioplasty / Stenting
- Arterial Thrombolysis
- Venous Thrombolysis
- Deep venous Embolectomy
- Sclerotherapy for anterio-venous malformation
Pain Management in Oncology
To improve the quality of life of the cancer patients, various image guided procedures are carried out
- Image Guided nerve Blocks like Coeliac Plexus Block, Stellate Ganglion Block
- Vertebroplasty, Kyphoplasty
- Transarterial Embolisation
- Radiofrequency Ablation
THROMBOSIS MANAGEMENT IN ONCOLOGY
Thrombosis Management in Oncology:
Thrombosis of various veins and arteries is a quite prevalent for oncology patients.
IR unit plays an active role in management of these conditions with procedures like;
- Deep Vein Thrombolysis / Embolectomy
- Pulmonary Thrombolysis / Embolectomy
- Intracranial Venous Sinus Thrombolysis
- SVC / IVC Filter Placement and Retreival
- Portal vein Thrombolysis
Training and Education
Post graduate degree (MD), DM and fellowship courses in Radiodiagnosis affiliated by the Homi Bhabha National Institute (HBNI) are offered by the department
The department is recognized by MCI as a teaching department for 17 candidates for MD (Radiodiagnosis) courses, 2 candidates for DM (Interventional Radiology) courses and 1 candidate for Fellowship in Oncoimaging annually.
Residency Programme
Post graduate students who are registered for the MD course at TMH enter the residency programme of 3 years duration for MD students. Admission to MD course is through NEET.
We have 2 seats for DM course in interventional radiology started from year 2017. It is a 3 years course in interventional radiology and interventional oncoradiology. Admission to the DM course is through NEET.
Fellowships in oncoimaging is a 2 years course. For it, MD/DNB qualification in Radiodiagnosis is required and admission is through a written examination followed by an interview.
For Senior Registrars posts (non bonded candidates), a MD or DNB qualification in Radiodiagnosis is required, and candidates are selected at an interview on the basis of their qualifications and experience. The SR posts are of 1 year duration, and can be extended upto 3 years.
The SR posts commence on 1st February and 1st August each year, and are advertised 2-3 months in advance.
Observers
Qualified Radiologists are also accepted as Observers in the department for short term training of 2 weeks to 6 months duration in specific areas of oncoimaging (viz mammography, CT, MRI) and interventional radiology.
Technician Training Program
We offer a two year full time course 'Advanced Diploma in Medical Imaging Technology' for the radiology technologist after graduation from B.Sc and B. pharma stream. This is affiliated with the Maharashtra State Board of Technical Education. We offer 20 seats per year
Research
The staff members of the Dept. of Radiodiagnosis are participating in more than 50 multidisciplinary clinical research projects. We have recently introduced TNM staging app to help clinicians to evaluate and stage the disease. The thrust areas of clinical research are:
• Evaluation of the accuracy of MDCT scanning in staging of gastric cancer
• Evaluation of accuracy of MRI in staging of cancers of rectum, cervix, endometrium and prostate.
• Evaluation of new radiotherapeutic and chemotherapeutic protocols in the treatment and follow up of brain and bone tumours, and cancer of cervix using Magnetic Resonance Imaging.
• Ultrasound evaluation of neck node metastases in carcinoma of lung, oesophagus, and head & neck tumours.
• Assessment of the impact of mammography on early detection of breast cancer and survival of patients diagnosed to have breast cancer.
• Participation in new drug trials for the treatment of recurrent or metastatic breast cancer and head & neck cancer, employing ultrasound, CT and MRI scanning in the evaluation of response to chemotherapy.
• Evaluating the efficacy of Radiofrequency ablation of hepatic neoplasms.
• Evaluation of efficacy of Radiofrequency Ablation in Osteoid osteoma.
• Evaluation of efficacy of Radiofrequency Ablation in fibromatosis.
• Locoregional therapies in hepatocellular carcinoma.
• Safety and Efficacy Evaluation of Superselective Ophthalmic Artery Chemoinfusion (SOAC) for Intraocular Retinoblastoma.
• Utility of Robotic arm and planning system for CT guided biopsy.
• To study the incidence and trend of the incidentalomas of adrenal gland.
• Cavitation, Attenuation, Ground Glass Opacity Components Evaluation with RECIST (CAGE RECIST): Impact on Objective Response Evaluation of Chemotherapy in NSCLC.
• The Diagnostic Performance of Thyroid Multimodal- imaging Comprehensive Risk Stratification Scoring (TMC-RSS) In Characterizing Thyroid Nodules.
• Effects of body composition as measured by CT on clinical outcomes in patients with oesophageal and lung cancer.
• MR imaging features and its correlation with molecular alterations in driver oncogenes in NSCLC patients with Brain metastasis.
We have been in collaboration with various institutes and universities for research and developmental activities.
1. Predible Health Pvt. Ltd for development of radiogenomics research, image analysis and deep learning solutions using radiology and genomic data since September 2017
2. Institute for Plasma Research,Gandhinagar for development of an artificial intelligence software for automated classification of chest X- Rays since January 2017.
3. Martino Centre for Biomedical Imaging at Massachusstes General Hospital, Boston, MA. USA an affiliated teaching hospital of the Harward Medical School for
a. Advanced image cooperation shall be focused on
b. Development of quantitative imaging biomarkers and radionics features
c. Development and validation of open source tools being developed at MARTINOS as part of our participation in NCI’s quantitative imaging network (QIN) on data acquired at TMH.
4. National Cancer Institute of the National Institute of Health, since January 2014 for
a. To evaluate hypoxia imaging methods in newly diagnosed cervical cancer
b. To develop quantitative novel hypoxia – and hypoxia signaling-specific molecular biomarkers and imaging methods
c. Assessing outcome and assessing correlation with hypoxia application of these techniques in studying cervical cancer biology and devising improved treatments.
5. Shri Guru GobindSinghji Institute of Engineering and Technology, Nanded since May 2016 for
a. To conduct joint/collaboration research and consultance in the areas of medical image processing like early stage cancer detection and diagnosis imaging quantification of body composition in cancer patients etc. Also validation of software being developed at SGGSIE&T as part of research work.
b. To collaborate to share and exchange information of National level projects between both the parties for mutual benefit and knowledge enhancement. To increase the relevance of academics research (Joint guidance for Ph. D and PG students) and product development initiatives
6. G. Narayanamma Institute of Technology and Science (for women), Hyderabad since May 2016 for
a. To conduct joint/collaboration research and consultance in the areas of medical image processing like early stage cancer detection and diagnosis imaging quantification of body composition in cancer patients etc. Also validation of software being developed at GNITS as part of research work.
b. To collaborate to share and exchange information of National level projects between both the parties for mutual benefit and knowledge enhancement. To increase the relevance of academics research (Joint guidance for Ph. D and PG students) and product development initiatives.
All the patients coming to the Radiodiagnosis department should follow these instructions.
- Avoid areas where direct radiation exposure is happening as mentioned in the department through prominent signboards.
- All pregnant patients should refrain from the areas of radiation mentioned in the department through prominent signboards.
- For women in reproductive age groups, the investigations which involve radiation exposures (e.g., x-rays, CT, Fluoroscopy), should be preferably carried out during 1st 10 days of menstrual cycle to avoid exposure to possible conceptus.
Patients should bring all previous studies (including CDs, films, and reports of previous imaging) while coming for radiological investigations.
- One relative should accompany the patient.
- Patient has to take prior appointment for USG and color Doppler, CT scan, MRI, biopsy and FNACs and interventional procedures. No prior appointment is generally required for radiography (x-rays) and Mammography.
Patient preparation
For Radiography:
- For chest and skeletal radiography and barium/conray swallow, sialogram, sinogram, Micturating Cystourethrogram (MCU) and Retrograde Urethrogram (RGU)- No preparation is required.
- For abdomen x-rays including KUB, barium enema, barium meal follow through and IVP (Intravenous Pyelogram)- Bowel preparation is required.
Bowel preparation:
- 2 days pre medication with Tab. Dimol (2TDS) and Tab. Dulcolax (2HS) (except for those patients having diarrhea) is required with low fiber diet. Overnight fasting is required the day before the examination. X-ray is performed in early morning on empty stomach. Patients can however drink water and take any routine medications they are on.
- For Loopogram- Stoma wash is required before and after the procedure.
For Mammography:
- Avoid the use of talcum powder and deodorant over breast and axilla.
- No other specific patient preparation is required.
For Ultrasonography (USG) and Doppler:
- 4 hours fasting is required for USG of Abdomen and color Doppler study of abdomen.
- No fasting is required for USG of chest, breast, neck, extremity and small parts as well as transrectal and transvaginal ultrasound.
- For KUB and pelvis, full bladder is required.
- Bowel preparation is required for Doppler study of abdomen.
For Computed Tomography (CT) scan:
- 4 hours fasting is required.
- Patient should have recent serum creatinine report. Serum creatinine report within 15 days will suffice for outpatients. For inpatients, a recent 2-day serum creatinine is preferred.
- History of allergy
-If patient has history of allergy to prior CT contrast media or has active asthma, this should be informed to the doctor before undergoing CT scan, as well as to the person giving the appointment at the time of taking CT appointment.
-If after CT scan, patient develops rashes, nausea, vomiting, facial edema, swelling at site of contrast injection, breathlessness, tachypnea, syncope, should be immediately informed to the doctor.
- For diabetic patients, if on metformin, there is no need to stop it if eGFR >30. If the eGFR measures <30, it should be stopped for 48 hours after the CT.
- Patients with high blood pressure can continue anti-hypertensive medications.
For Magnetic Resonance Imaging (MRI):
- If patient has history of any implant (like pacemaker, cochlear implant, insulin pumps etc.), should be informed to the doctor before entering into the MRI.
- Patient should not carry any metallic objects into the MRI scanning room.
- 4 hours fasting is preferred if contrast MRI is required. For non contrast MRI, no fasting is required (except for MRCP).
- Patient should have recent serum creatinine report. Serum creatinine report within 15 days will suffice for outpatients. For inpatients, a recent 2-day serum creatinine is preferred.
- Diabetic patients and patients with high blood pressure can continue their medications.
For CT and USG Guided biopsies and FNACs:
- 4 hours fasting is required for all biopsies and FNACs except for USG guided FNAC and biopsy of superficial lesions likely thyroid, breast, extremities, neck, etc.
- Blood investigations required- Complete blood cell count (CBC), Coagulation profile, Renal Function test (for CT guided biopsy and FNAC only).
- For TRUS guided biopsies- premedication is required as follows.
-Tab. Dimol (2TDS) and Tab. Dulcolax (2HS) (Except in those patients having diarrhea) for 2 days before biopsy and with low fiber diet. Overnight fasting is required the day before biopsy.
-Tab. Norflox TZ (1BD) 2 days before and 3 days after biopsy.
We are introducing online quiz in radiology every month. Case calendar coming soon...
 Department Office Number: (+9122) 24177000 / Ext.No.4157
Department Office Number: (+9122) 24177000 / Ext.No.4157
 Department of Radiodiagnosis ,Ground Floor,Main Building,
Department of Radiodiagnosis ,Ground Floor,Main Building,
TATA MEMORIAL HOSPITAL, Dr.E.Borges Road, Parel, Mumbai-400-012
Maharashtra, India
 Hospital Fax Number: (+9122) 24146937
Hospital Fax Number: (+9122) 24146937
 Email-id: radiology@tmc.gov.in
Email-id: radiology@tmc.gov.in
- Anesthesia
- Biochemistry
- Cancer Cytogenetics
- Cytopathology
- Dental Services
- Digestive Diseases
- General Medicine
- Hemato-Pathology
- Medical Oncology
- Medical Physics
- Microbiology
- Nuclear Medicine
- Nursing
- Pathology
- Palliative Medicine
- Preventive Oncology
- Pulmonary Medicine
- Radiation Oncology
- Radiodiagnosis
- Surgery
- Transfusion Medicine
Our Expertise Network for
All Departments
बार-बार देखा गया
ग्लोबल नेविगेशन
हमसे संपर्क करें
टाटा स्मारक अस्पताल
डॉ ई बोर्जेस रोड, परेल, मुंबई - 400 012 भारत
फ़ोन: +91-22- 24177000, 24146750 - 55
फैक्स: +91-22-24146937
ईमेल : msoffice@tmc.gov.in (रोगी देखभाल और प्रश्नों के लिए) / hrd@tmc.gov.in(प्रशासनिक के लिए - HRD मायने रखता है)
कॉपी राइट © 2016 टाटा स्मारक केंद्र, को है. सभी अधिकारी सुरक्षित.इस वेबसाइट को सबसे अच्छी तरह देखा जा सकता है फ़ायरफ़ॉक्स,माइक्रोसॉफ़्ट एक्सप्लोरर 9.0+, Chrome, फ़ायरफ़ॉक्स


द्वारा परिकल्पित एवं विकसित ग्लोबलअॅप