- Online Patient Services
- Patient Booklet
- e - Medical Records
- Online Expert Opinion-NAVYA
- Donation to TMC
- Online Hospital Statistics
- Pensioner Portal
- Travel Facility
- Schedule of Charges
- FAQs
- International Patients Advisor
- TMC - Annual Report
- TMC -Performance Statistics
- TMH Facts: average per day
- Classification of Surgeries
- D.A.E
- Govt of India Sites :
- International Affiliations
- Pancreatic Cancer India
- Tobacco Act
- Observership Application
- Teleconsulting Services
- TMC
- Home
- About Us
- Cancer Information
- Patient Services
- Departments
- NCG
- Disease Management Group
- Education and Research
- Events
Paediatric Solid Tumours
- Members
- Service
- General Information
- Education
- Research
- News & Events
- Contact Us
Convener : Dr. Maya Prasad ( Medical Oncology )
Secretary : Dr. Mukta Ramadwar ( Pathology )
Medical Oncology
- Dr. Girish Chinnaswamy
- Dr. Maya Prasad
- Dr. Badira Cheriyalinkal Parambil
- Dr. Venkata RamaMohan Gollamudi
Radiation Oncology
- Dr. Siddhartha Laskar
- Dr. Nehal Khanna
- Dr. Jifmi Jose Manjali
Surgical Oncology
- Dr. Sajid Qureshi
Nuclear Medicine and Molecular Imaging
- Dr. Venkatesh Rangarajan
- Dr. Sneha Shah
Radiologist
- Dr. Suyash Kulkarni
- Dr. Akshay Baheti
- Dr. Kunal Gala
- Dr. VasundharaPatil
Physiotherapy
- Ajeeta Kulkarni
- Sarika Mahajan
Honorary
- Dr. Nandan Shetye - Ophthalmology
- Dr. Sudha Rao - Endocrinology
- Dr. Anurag Shrimal- Liver & Pancreas Transplant
Pathologist
- Dr. Mukta Ramadwar
- Dr. Poonam Panjwani
Palliative Care
- Dr. Maryann Muckaden
- Dr. Joyita Deodhar
- Dr. Shamali Poojary
Department of Anesthesia
- Dr. Bhakti Trivedi
- Dr. Jeson Doctor
- Dr. Madhavi Desai
- Dr. Nayana Amin
- Dr. Shilpushp Bhosale
Clinical Pharmacology
- Dr. Vikram Gota
Financial/Support support
- Ms. Shalini Jatia
- Ms. Ameeta Bhatia
Occupational Therapy
- Dr. Manjusha Vagal
Trial Coordinator
- Dr. Amey Paradkar
Psychiatry and Clinical Psychology
- Mrs. Savita Goswami
Services
The Paediatric Solid Tumour Disease Management Group (PST DMG) caters to children (<15 years) with extracranial paediatric solid tumours. The team consists of specialists from the field of paediatric oncology, paediatric surgery, paediatric radiation oncology, ophthalmology, pathology, radiology (including intervention radiology), nuclear medicine and palliative care medicine. Current members are as above.
Outpatient Services
All Paediatric Medical Oncology OPD suites (both for general as well as private category patients) are situated on the Ground Floor in the Main Building. Patients are seen on all working days of the week (Monday to Saturdays). Beyond working hours, on holidays and in case of emergencies, patients are seen in the Casualty located on the Ground Floor of the Main Building.
OPD Timings for pediatric Solid Tumor OPD
Paediatric Medical Oncology: 09:30 am –6:00pm from Monday to Friday, and 10am -2:00 pm on Saturday; OPD 80, Ground Floor , Main Building
Paediatric Surgical Oncology: 09:30 am –6:00pm from Tuesday, Friday; OPD 80, Ground Floor, Main Building.
Paediatric Radiation Oncology: 08:30 am –4:30 pm Monday, Tuesday, Wednesday Friday; OPD 93, Ground Floor, Main Building.
Speciality Clinics:
Endocrinology Clinic: Wednesday 3.00 pm-7.00pm OPD 80
Ophthalmology Clinic: Tuesdays 10.00 am-12.00 noon OPD 80
Dermatology Clinic: Wednesdays 10.00 am-12.00 noon OPD 80
After Completion of Treatment Clinic: Tuesdays and Thursdays 9.00 am -5.00 pm OPD 84
Inpatient Services
The 44-bedded paediatric ward on 11th floor of Annexe building is common to paediatric haemato-lymphoid and paediatric solid tumour DMGs, including post-operative patients. Private category patients are admitted in the private/semiprivate wards in the Homi Bhabha Building and Main Building. Critically ill patients are admitted in the intensive care unit where patients are managed by intensivists trained in paediatric critical care.
Daycare Services
Paediatric patients received chemotherapy and supportive care in the paediatric general day care on the 9th floor of Annexe building, and a separate bay in private day-care, manned by paediatric oncology nurses and a pharmacist employed by our division.
Patient registrations (Paediatric Solid Tumour DMG) for the year 2023- 666
General Information
PST DMG works closely with the paediatric haematolymphoid DMG, and the paediatric component of Bone and Soft Tissue DMG and Neuro Oncology DMG.
The paediatric oncology division (including PST DMG) prides itself on the holistic support strategy for over a decade. The division has a dedicated team of infection control nurses, paediatric nutritionists, clinical psychologist, medical social workers and volunteers. Both paediatric OPDs (paediatric haemato-lymphoid and paediatric solid tumour OPD) function in adjoining areas. All patients receive support in terms of emergency funds, accommodation, nutrition, infection counselling and other support within the first week.
Patients from the PST DMG are also managed at the paediatric oncology OPD and 12-bedded ward at ACTREC
Patients are managed as per National Cancer Grid Guidelines for Paediatric Cancers
https://tmc.gov.in/ncg/docs/PDF/Breast/NCG_GUIDELINES_2020_Pediatric_Oncology.pdf
Education
Current training programs include DM (intake 6/year) and HBNI fellowships (intake 2/year) in Paediatric Oncology. There are 1-year fellowships in Paediatric Surgical Oncology and Paediatric/ BST radiology. Trainees in MCh Surgical Oncology,MD Palliative medicine, Radiation Oncology, Pathology etc rotate through PST DMG services.
The DMG also accommodates several national and international observers.
Research
Over the past 5 years, the PST DMG has conducted 20 prospective/interventional studies which enrolled 3983 patients, as well as 38 retrospective studies
Events in 2016/2017
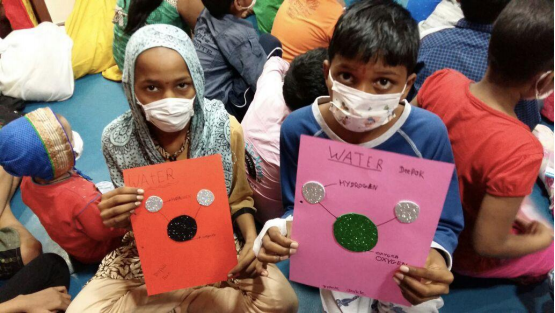
ImPaCCT Foundation School Program




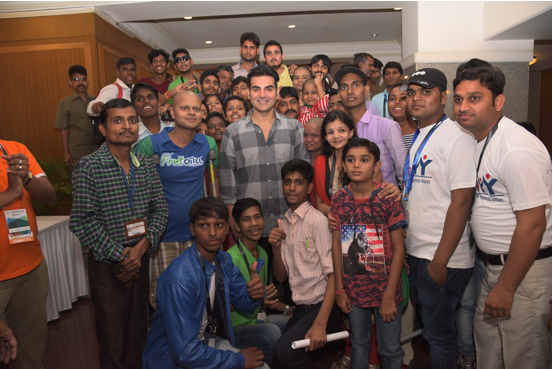
Annual event Hope 2016




Pediatric Birthday celebrations
Moscow Trip 2017




Parent Support Group Meetings
OPD workshops
Visit by the Clown




2nd Annual Paediatric Workshop-2017




TYCON Conference-2017




 Department Office Number: (+9122) 24177000 / Ext.No.- 7204
Department Office Number: (+9122) 24177000 / Ext.No.- 7204
 Department of Pediatric Solid Tumours,
Department of Pediatric Solid Tumours,
TATA MEMORIAL HOSPITAL, Dr.E.Borges Road, Parel, Mumbai-400-012
Maharashtra, India
 Hospital Fax Number: (+9122) 24146392
Hospital Fax Number: (+9122) 24146392
 Email-id: dmgpae@tmc.gov.in , prasadm@tmc.gov.in
Email-id: dmgpae@tmc.gov.in , prasadm@tmc.gov.in
Frequently Visited
Global Navigation
Contact Us
TATA MEMORIAL HOSPITAL
Dr. E Borges Road, Parel, Mumbai - 400 012 India
Phone: +91-22- 24177000, 24177300, 69537300
Fax: +91-22-24146937
E-mail : msoffice@tmc.gov.in(for patient care and queries)/cash@tmc.gov.in(for accounts related)/fundraising@tmc.gov.in (for donors and donation related)/registrar@tmc.gov.in(for education and training)/hrd@tmc.gov.in(for administrative - HRD matters) This email address is being protected from spambots. You need JavaScript enabled to view it.
Copyright © 2016 Tata Memorial Centre. All rights reserved.This website can be best viewed in Microsoft Internet Explorer 9.0+, Chrome, Firefox


Designed and Developed by Mindspace Software Technologies Pvt. Ltd.