- Online Patient Services
- Patient Booklet
- e - Medical Records
- Online Expert Opinion-NAVYA
- Donation to TMC
- Online Hospital Statistics
- Pensioner Portal
- Travel Facility
- Schedule of Charges
- FAQs
- International Patients Advisor
- TMC - Annual Report
- TMC -Performance Statistics
- TMH Facts: average per day
- Classification of Surgeries
- D.A.E
- Govt of India Sites :
- International Affiliations
- Pancreatic Cancer India
- Tobacco Act
- Observership Application
- Teleconsulting Services
- TMC
- Home
- About Us
- Cancer Information
- Patient Services
- Departments
- NCG
- Disease Management Group
- Education and Research
- Events
Head & Neck Services
- Members
- Services
- Meetings / OPD
- Teaching & Training
- Research
- News & Events
- Patient Information
- Contact Us
Convener: Dr. Sarbani Ghosh Laskar (Radiation Oncology)
Secretary: Dr. Asawari Patil ( Pathology )
Surgical Oncology
- Dr. Anuja Deshmukh
- Dr. Arjun Singh
- Dr. Deepa Nair
- Dr. Gouri Pantvaidya
- Dr. Pankaj Chaturvedi
- Dr. Poonam Joshi
- Dr. Prathamesh Pai
- Dr. Rathan Shetty
- Dr. Richa Vaish
- Dr. Shiva Kumar Thiagarajan
- Dr. Sudhir Nair
- Dr. Vidisha Tuljapurkar
Radiation Oncology
- Dr. Anuj Kumar S
- Dr. Ashwini Budrukkar
- Dr. Monali Swain
- Dr. Sarbani Ghosh Laskar
- Dr. Shwetabh Sinha
Nuclear Medicine
- Dr.Archi Agarwal
- Dr.Nilendru Purandare
- Dr.Sneha Shah
- Dr.Venkatesh Rangarajan
Radiology
- Dr. Amit Janu
- Dr. Arpita Sahu
- Dr. Kajari Bhattacharya
- Dr. Nivedita Chakarbarty
- Dr. Suman Kumar Ankathi
- Dr. Vasundhara Patil
Plastic & Reconstructive
- Dr. Ameya Bindu
- Dr. Dushyant Jaiswal
- Dr. Mayur Mantri
- Dr. Saumya Mathews
- Dr. Vinaykant Shankhadar
- Dr. Vineet Pilania
Pathology
- Dr. Asawari Patil
- Dr. Katha Kante
- Dr. Munita Bal
- Dr. Neha Mittal
- Dr. Swapnil Rane
Cancer Biology
- Dr. Amit Dutt
- Dr. Manoj B. Mahimkar
- Dr. Murali K. Chilakapati
- Dr. Sanjiv Waghmare
- Dr. Sharada Sawant
- Dr. Tanuja Teni
Physiotherapy Department
- Anuradha Daptardar
- Sarika Mahajan
Medical Oncology
- Dr. Amit Joshi
- Dr. Kumar Prabhash
- Dr. Nandini Menon
- Dr. Vanita Noronha
- Dr. Ajaykumar Singh
Dental & Prosthetic Surgery
- Dr. Gurkaran Preet Singh
- Dr. Madhura Sharma
- Dr. Sandeep Gurav
Speech & Swallowing Therapist
- Mr.Arun Balaji
- Mr. Rukmangathan T M
- Madhura Bhalerao
DMG Coordinator
- Ms. Indumati Mhatre
- Ms.Nasirintara Shah
ENT Surgeon
- Dr. Chris D'souza
Audiologist
- Mr. Jitesh Sahoo
Occupational Therapist
- Dr. Manjusha Vagal
- Dr. Rebeka Marri
HN cancers constitute 25% of the annual registrations at TMC. The DMG comprises of major oncology specialists (Surgical, Radiation and Medical oncology), effectively supported by other ancillary and rehabilitative services, providing effective, evidence based care for HN cancer. The activities are grouped as SERVICE, EDUCATION, and RESEARCH.
Service
Multi disciplinary Joint Clinic (JC) to suit the individual treatment decision is held daily. All newly diagnosed patients, worked up patients are evaluated in this clinic. The plans are evidence based adhering to our as well as international guidelines. This is new registration details for past 6 years.
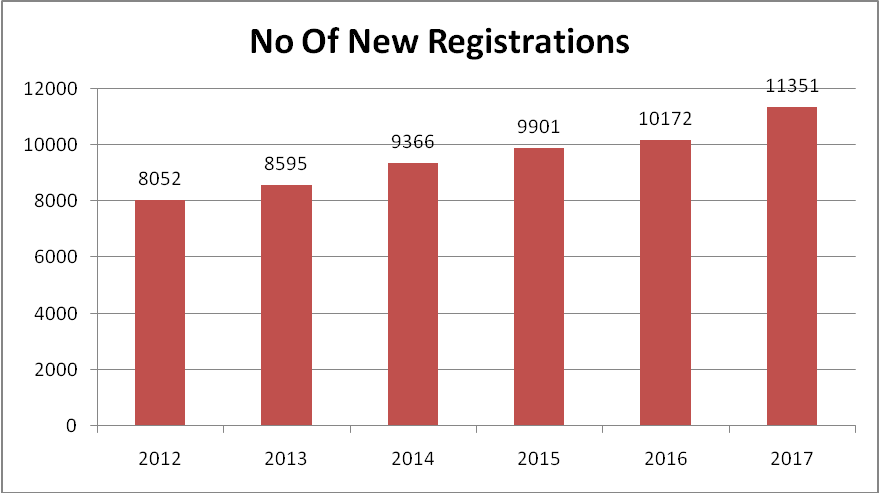
Registrations in HN Cancers 2012-2017 (2.73% increase this year)
Our Specialized Services:
- Skull Base surgery
- Robotic surgery
- Laser surgery
- Micro vascular reconstruction
- Speech and Swallow rehabilitation
- Dental rehabilitation
OPD Timings
General OPD – Monday - Friday
Monday & Wednesday- Head and Neck Unit B
Tuesday & Friday – Head and Neck Unit A
Tuesday & Thursday- Head and Neck Unit C
Timing - 09:15-17:30 Hours, Saturday, Timings 09:15-13:00 Hours
Location -1st Floor, Golden Jubilee Building ,Room No. 107.
Private OPD - Monday - Friday
Monday & Wednesday- Head and Neck Unit B
Tuesday & Friday – Head and Neck Unit A
Tuesday & Thursday- Head and Neck Unit C
Timing - 09:15-17:30 Hours, Saturday, Timings 09:15-13:00 Hours
Location 2nd Floor, Homi Bhabha Building -Room No.210.
Surgical Oncology
Education
The department of head neck surgery has been in the forefront of education in the field of head neck oncology. It was the first department in the country to start the head and neck MCh surgical oncology programme from the year 2013. This is a structured training programme over a span of four years that enables students to become masters in the field of head and neck surgery. It is a comprehensive teaching programme that encompasses training in surgical skills including advanced skills in endoscopic, microvascular, robotic and laser surgeries. The department of HN surgery encourages and guides students to write research protocols and carry them through to practice changing conclusions and peer reviewed publications.
The teaching programme is a structured programme consisting of weekly bedside teaching along with didactic lectures and case presentations. A multidisciplinary joint clinic led by a head and neck surgeon is held each day where residents, fellows and trainees present and discuss head and neck cancer cases.
A bedside clinical grand round is conducted every Thursday which is attended by all residents and students across the 3 subunits in the department. This teaching round is conducted by all surgical faculties in rotation. This helps students in understanding various viewpoints and in maintaining uniformity of resident education.
Skull Base Clinic is run by the service every Thursday afternoon at 3.00 pm. Skull base tumours are managed by a multi-disciplinary team consisting of Head & Neck surgeons, Neurosurgeons, Radiation Oncologists, Medical Oncologists, Radiologists and Interventional radiologists.
A didactic teaching programme discussing management aspects of various head and neck cancers is held biweekly throughout the year. This is in the form of seminars where student’s present evidence based management guidelines on treatment aspects of various cancers in the head neck. This platform also allows residents to discuss new ideas in clinical and translational research.
The department takes pride in hosting approximately 70-100 national and international observers each year. The observers attend the multidisciplinary joint clinics and participate in joint discussions allowing a two way transfer of knowledge.
Surgeons from department of surgery are well renowned and are at the helm of teaching programmes and CMEs across the country and internationally.
Courses
Trainings & Fellowship -The DMG trains many doctors of different specialities from all over India in Head and Neck oncology to meet the increasing need in this country.
- Ch Head and Neck Surgery: This has been initiated since 2013. 4 students are enrolled every year.
- HBNI Fellowship for two years.
- Sekhsaria Fellowships -3 Students each year. It is one year sponsored fellowship
- Surgical Oncology Training for 6 months
- International Head & Neck Surgical Fellowship
Medical Oncology
Education
The medical oncology students have a well charted program for clinical & research related education.
Clinical education
A teaching class is taken on Tuesday, Wednesday, Thursday and Saturday of one hour. The program consists of discussion of difficult cases, seminars, short reviews, case presentation and journal clubs. Both faculty and residents participate in the program.
The program is designed ion 3 fold basis
- Coverage of basic of cancers and chemotherapy (Dealt mainly in Saturday classes)
- Coverage of clinical skill and history presentation (Dealt mainly in Wednesday’s class)
- Coverage of head and neck related trials and its application in practice (dealt mainly on Tuesday and Thursday)
Research education
The students are sensitized towards research. They are given an overview of studies running in department. In OPD they actively screen patient for it. Every student is given a small project or a retrospective analysis so that he understands the intricacy of doing research. Research methodology related classes are taken.
Laboratory exposure is provided to students on Friday. The test used in Medical Oncology translational lab is briefed and an opportunity for hands on experience is given.
These researches related activities are done on Friday and Thursday.
Courses
Audit of systemic therapy planning on Tuesday and Thursday.
Training – All DM medical oncology fellows gets training in Head and Neck oncology to meet the increasing need in this country.
Radiation Oncology
Education
MD(Radiotherapy): 3-year course, during which every student rotates through head and neck for a period of 3 months, at least. In addition, the students also spend 3 more months as senior registrar.
The department also gets Fellows and Observers from other Oncology Institutes in the country and neighboring countries. We do get a good number of observers for brachytherapy and precision radiotherapy.
The department also offers a 2 year HBNI Fellowship programme in IMRT-IGRT.
Courses
Seminars & planning meets are held in Radiation Oncology every Monday & Friday. In addition planning meetings are held regularly.
Research
Research within the DMG focuses on evaluating standards of care in randomized settings, challenging dogma and evaluating new technology/ drugs and has the potential of generating high quality evidence to support translation into standard of care. The DMG members actively participate in National and International multicentric trials and have been responsible for conceptualizing, designing and implementing several prospective trials with either intramural or extramural support. The DMG members also participate in trials supported by the pharma. The DMG also has several ongoing basic science and translational research studies
- Translational research – carcinogenesis, immunology, proteomics, gene therapy etc
- Oral cancer screening, prevention and early detection
- Extent of treatment - extent of Neck dissection in clinically N0 neck, adjuvant treatment of high risk oral cancers, management of advanced larynx/hypo pharynx cancers.
- Quality of Life
- Comprehensive Rehabilitation
- Evaluation of high precision radiotherapy techniques: IMRT/ IMRT-IGRT.
- Development of low cost, indigenous immobilization devices for radiotherapy.
- To develop low cost systemic therapy in head and neck cancer. (e.g.- metronomic therapy)
Each faculty member is leading one of the above as their area of interest. We are the only DMG to appoint a dedicated clinical scientist in our service to give impetus to translational research.
Overview of clinical trials in the year 2016 in TMH & ACTREC
|
|
Total number of clinical trials |
Completed Trials |
Ongoing Trials |
Overall Patients Accrued |
|||
|---|---|---|---|---|---|---|---|
|
|
Investigator Initiated |
Sponsored Initiated |
Investigator Initiated
|
Sponsored Initiated |
Investigator Initiated |
Sponsored Initiated |
|
|
TMH |
22 |
2 |
12 |
0 |
31 |
2 |
1958 |
|
ACTREC |
13 |
0 |
7 |
0 |
33 |
0 |
|
|
Total |
35 |
2 |
19 |
0 |
61 |
2 |
|
|
Grand Total |
37 |
19 |
64 |
||||
Practice changing trials with their significance
|
Sr No |
Trial Title |
Why is it Practice changing Trial? |
|---|---|---|
|
1 |
Elective versus Therapeutic Neck Dissection in the treatment of early node negative squamous cell carcinoma of the oral cavity |
The management of neck in early oral cancers is a contentious issue. The trials had small sample sizes and even the meta-analysis published by Fasunla et al in 2011failed to impact on clinical practice with the debate still persisting. |
|
2 |
Phase III trial of surgery followed by conventional radiotherapy (5 fractions/ week) vs concurrent chemoradiotherapy vs accelerated radiotherapy (6 Fractions/week) in high risk, locally advanced stage III & iva, resectable, squamous cell carcinoma of oral cavity |
Results of the trial will help in deciding whether treatment intensification is necessary in the presence of high risk factors in the adjuvant setting. The trial will also answer the question on the optimal method for treatment intensification. |
|
3 |
Phase II Study Of 3-Dimensional Conformal Radiotherapy (3D-CRT) Vs.Intensity Modulated Radiotherapy (IMRT) For Squamous Cell Carcinoma Of The Head & neck (HNSCC) |
IMRT resulted in significantly lesser incidence and severity of xerostomia (both acute & late) compared to 3D-CRT in definitive (chemo) radiotherapy of HNSCC with better preservation of QOL without any detrimental impact upon loco regional control or survival. Both these RCTs ran in parallel at TMH & ACTREC and were designed even before the PARSPORT study (N=84) from UK, which was hailed as a landmark publication (a year earlier to our results). Our data has also been included in a subsequent meta-analysis that clearly established the superiority of IMRT over 2D/3D-CRT. |
|
4 |
The role of neoadjuvant chemotherapy for mandibular preservation in locally advanced operable squamous cell carcinoma of the oral cavity |
A study by TMH demonstrated that only 40% of the mandibles resected are actually involved by tumor. A significant number of mandibles are resected due to paramandibular soft tissue disease. |
|
5 |
A randomized trial comparing intensity modulated external beam radiation alone vs intensity modulated radiation and brachytherapy for reduction in xerostomia in patients with early staged oropharyngeal cancers |
This phase II randomised trial is planned to compare IMRT alone vs IMRT+ Brachytherapy for early stage oropharyngeal cancer with xerostomia reduction as the primary end point. This trial is much looked forward to in the head neck brachytherapy circles. This is the ONLY ongoing trial in the entire world which will answer important question of additional advantage of brachytherapy over IMRT and hence will be practice changing. |
|
6 |
Effect Of COX-2 and EGFR Suppression On Molecular Markers Of Angiogenesis And Proliferation In Squamous Cell Carcinoma Of Oral Cavity – A Prospective Randomized Study |
1.A Molecular Signature that can predict response to EGFR TKIs and help in selecting suitable patients. 2.Understand the impact of combining two targeting agents that can be administered orally and having less known side effects. 3.Will down staging tumours have potential impact on extent of resection and morbidity |
|
7 |
An Open label, Randomized, Investigator Initiated Multicentric, Phase III Study of Nimotuzumab in combination with Concurrent Radiotherapy and Cisplatin versus Radiotherapy and Cisplatin alone, in Subjects with Locally advanced Squamous Cell Carcinoma of the Head and Neck (LASCCHN) |
Inspite of improvement in survival in head and neck cancer long term survival remains approximately 40% suggesting huge unmet need. There is enough data to suggest that EGFR inhibitors works in head and neck cancer. Nimotuzumab has been investigated in phase II study ( 90 patients) which met its primary endpoint. This study suggested that nimotuzumab in combination with chemo-radiation improves response rate and PFS and OS. This phase II trial was not powered for OS. This present study is a investigator initiated study to confirm the finding of the phase II study. |
|
8 |
A prospective randomized phase II Study comparing metronomic chemotherapy with chemotherapy (single agent cisplatin),in patients with metastatic, relapsed or inoperable squamous cell carcinoma of Head and Neck |
No chemotherapy has evrer shown to improve survival in head and neck cancer except cetuximab based therapy which only 1-2 % of our patients can use. This is the first time that a study has shown that chemotherapy can improve RR, PFS QOL AND OS in this setting. This is a small randomized trial but well powered for PFS. This has leaded to change in the practice in our hospital where significant proportion of patients are now administered oral chemotherapy based on this study. As compared to a situation where there was no standard treatment. |
|
9 |
A randomized trial comparing oral metronomic chemotherapy vs IV chemotherapy in palliative setting of head and neck cancer. |
We have completed a phase II study with similar design and now this is a Phase III study with OS as a endpoint. |
|
10 |
Phase III non-inferiority randomized trial comparing three-weekly Cisplatin versus weekly Cisplatin in combination with radiation therapy in patients with advanced carcinoma of the head and neck |
The standard of care for radical chemo radiotherapy for locally advanced head and neck squamous cell carcinoma is high-dose 3-weekly cisplatin; however this requires intensive supportive care and is associated with significant toxicity. In our setup as well as in the West, including in various RTOG trials, the concurrent chemotherapy has become low dose weekly cisplatin. However, weekly cisplatin has never been compared to 3-weekly cisplatin in a prospective randomized fashion, for efficacy and safety. In our trial, we hypothesize that weekly cisplatin concurrently with radical radiotherapy is non-inferior to 3-weekly cisplatin, with a primary endpoint of locoregional control |
|
11 |
Impact of comorbidity on outcome in head and neck cancer patients- A prospective longitudinal study. |
Apart from the patients performance status , tumor stage and treatment offered, existent comorbidities contributes to the causes of mortality in these group of patients In this study we will see the impact of comorbidity on overall survival in these patients with head and neck cancer. |
|
12 |
Randomised controlled trial assessing addition of neoadjuvant and maintenance oral metronomic chemotherapy to standard surgery and adjuvant therapy in Stage III/IV Operable Oral cancers |
Time to treatment is a major concern in most centers both developed and developing. This is due to constraints of resources and increasing patient load. This leads to tumor progression. The waiting period between treatments leads to tumor repopulation. This study addresses the waiting periods with novel treatment modality which is universally applicable, cost effective and almost not toxic. The results of this trial will change practice and improve disease free survival and will pave the way to future research for improving overall survival. |
|
13 |
Phase II Randomized Controlled Trial Of Postoperative Intensity Modulated Radiotherapy (IMRT) in Locally Advanced Thyroid Cancers |
This trial would provide the best available evidence defining the role of adjuvant radiation in locally advanced thyroid cancers. This subset of thyroid cancers are aggressive and very little has been done in the form of prospective research in this group of patients. To the best of my knowledge there is no such trials ongoing anywhere in the world addressing this issue |
|
14 |
Biological imaging before, during, and after Simultaneous Modulated Accelerated Radiation Therapy in head and neck squamous cell carcinoma (Bio-SMART) |
This study has helped us standardize hypoxia imaging in head neck cancers. We have also been able to study the spatio-temporal variation of hypoxia and characterize patterns of oxygenation during a course of definitive (chemo)radiotherapy which will guide us towards biologically optimized adaptive dose-painted IMRT |
|
15 |
Prophylactic antibiotics in operable oral cancer: short course versus prolonged course - a randomized control trial |
If the hypothesis is proved, short course preoperative antibiotics can become standard of care in our centre and across the country for operable oral cancer. This will significantly reduce costs to patient, potentially reduce hospital stay and reduce antibiotic resistance. |
|
16 |
Prevalence and Clinical impact of p16 |
The first part of the study has been completed and data analyzed. For the first time ever we have produced robust data of prevalence of HPV in non oral HNSCC in India. Moreover, its clinical impact and interaction with tobacco reveals that HPV testing may be useful in only a small minority of all patients of HNSCC in India. This has major service and resource planning implications. |
|
17 |
Effect of Progressive Resistive Exercise Training on shoulder joint range of motion operative Head and Neck cancer patients undergoing radiotherapy; a randomized trial. |
The largest Randomized trial of this kind ever, in a problem that is under diagnosed and underreported. The final analysis shows that PRET is significantly (statistically and clinically) in improving shoulder function post neck dissection and RT. This should clearly change practice! |
|
18 |
Development of a gene signature predicting cervical lymph node metastasis in Tongue squamous cell carcinoma (GSP -TSCC). |
The information gained from this study can lead to the development of a customized gene chip that can be used clinically for making treatment decisions. This can lead to development of a commercially viable tool which can be patented and marketed and has potential to bring in revenue to the Institution. |
Events Organized
Surgical Oncology
- Mastercourse in Oral Cancer Management and Cadaver Dissection Workshop
This was held on 22nd & 23rd July 2016.This two day program was designed to provide an overview of oral cancer and its management, emphasizing on the surgical management of the oral cancer. This was covered in the form of didactic lectures, surgical video demonstrations, interactive discussions and panels. Basics steps of surgery, appropriate approaches for different lesions, reconstruction and rehabilitation were discussed.
- Global Post-Laryngectomy Rehalibiltaion Academy Workshop
This course is an international course which is run by Netherlands cancer Institute –Amsterdam in Affiliation with Tata Memorial Hospital-Mumbai. In this all participants get opportunity to practice Hands-on with live patients prosthesis replacements and demonstration
- TMC Head & Neck Laser Course
The 3rd TMC Head Neck Laser Course is designed for imparting knowhow in the use of the laser in the management of Head Neck Cancers. This course included live surgery and hands on training in the art and craft of laser surgery. This was held on 3rd to 4th Dec 2017
- Oncosurg
The Head and Neck surgical department actively participated in the Annual surgical workshop Oncosurg, conducted by the department of surgical Oncology. It includes Live surgical demonstration of thyroidectomy, laryngectomy, parotidectomy and glossectomy with neck dissection.
Medical Oncology-To be added
- Molecular workshop (hands on) organized every 4 months in molecular technology
- Workshop organized for toxicity management of chemo radiation
Radiation Oncology
XV Annual TMH Radiotherapy Practicum “Adaptive Radiotherapy in Practice”
Adaptive Radiotherapy has become a buzz word in the field of modern Radiation Oncology.
The advent of new technologies and integration of the imaging modalities for radiotherapy planning and delivery has borne the concept of adaptive radiotherapy. Adaptive radiotherapy has a potential to improve the therapeutic ratio by modulating radiotherapy planning and delivery according to the changing relation of target volumes with normal tissue. There is great interest in its application in different cancer sites particularly in pelvic tumors (Prostate and Bladder cancers) and Head Neck cancers. While, Image guided Radiotherapy, which is commonly available in increasing number of centers
in India, forms the cornerstone of adaptive radiotherapy, routine use of adaptive radiotherapy is limited by the uncertainties in understanding of the workflow and challenges in methods of implementation.
It was included hands-on practical experience in Adaptive Radiotherapy with special focus on pelvic and head neck cancers. Radiation Oncologists, Medical Physicists, and Radiotherapy Technologists are expected to benefit from this workshop. Being a relatively new concept, this provides a good opportunity for delegates to understand the practical aspects of this new and exciting technology from expert international and national faculty. It was held on 1st-2nd September 2017
 Department Office Number: (+9122) 24177000
Department Office Number: (+9122) 24177000
Private OPD Ext.No. 6209,6210,6211,6212,6213,6214,6215,6216,6217 / MOBILE No. SR II/III: 22184, 22164, 22337, 22457, 22402
General OPD Ext.No 4521,4558,4564,4579,4580
MOBILE No. SR II/III: 22184, 22165, 22190,
 Department of Head & Neck Services,
Department of Head & Neck Services,
TATA MEMORIAL HOSPITAL, Dr.E.Borges Road, Parel, Mumbai - 400-012
Maharashtra, India
 Hospital Fax Number: (+9122) 24101656
Hospital Fax Number: (+9122) 24101656
 Email-id: dmghn@tmc.gov.in
Email-id: dmghn@tmc.gov.in
Frequently Visited
Global Navigation
Contact Us
TATA MEMORIAL HOSPITAL
Dr. E Borges Road, Parel, Mumbai - 400 012 India
Phone: +91-22- 24177000, 24177300, 69537300
Fax: +91-22-24146937
E-mail : msoffice@tmc.gov.in(for patient care and queries)/cash@tmc.gov.in(for accounts related)/fundraising@tmc.gov.in (for donors and donation related)/registrar@tmc.gov.in(for education and training)/hrd@tmc.gov.in(for administrative - HRD matters) This email address is being protected from spambots. You need JavaScript enabled to view it.
Copyright © 2016 Tata Memorial Centre. All rights reserved.This website can be best viewed in Microsoft Internet Explorer 9.0+, Chrome, Firefox


Designed and Developed by Mindspace Software Technologies Pvt. Ltd.